Bone Education
Osteoporosis
Osteoporosis is a disease that makes bones weak and fragile. It can occur due to increased bone loss, decreased bone formation, or both. With progressive bone weakening, a person is more likely to fracture without a major trauma (for example, while coughing, picking up a grocery bag, or after a simple fall). The most common sites of these so-called fragility fractures are the spine, hip and wrist. Fractures can have serious consequences and can result in major health complications, such as infection, prolonged immobility, increased risk for admission to a long care facility and even death. Studies suggest that approximately one in two women and one in four men age 50 and older will break a bone due to osteoporosis.
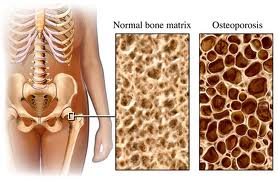
Before bones break, osteoporosis does not have any symptoms, so it is critical to know the risk factors for this disease and discuss screening tests available.
There are multiple risk factors that can increase a patient’s risk for osteoporosis:
- Family history of Osteoporosis or family history of fragility fracture
- Personal history of fragility fracture
- Smoking
- Heavy alcohol use
- Multiple medical conditions are implicated in bone loss including: rheumatological disorders, gastrointestinal disorders, epilepsy, cancer, COPD, premature menopause, hyperthyroidism, calcium disorders, eating disorders, liver disease, organ transplantations
- Medications causing bone loss include: long-term steroids, certain anti-seizure medications, excessive thyroid hormone, medications that are used to treat breast and prostate cancer, as well as anti-acid medications
- Bone Mineral Density (BMD) assessment by dual-energy x-ray absorptiometry (DXA) is the standard test to diagnose osteoporosis. As a screening test, it is indicated for women above the age of 65 and men above the age of 70, however, if you have any risk factors to develop osteoporosis or you have broken a bone, you should have DXA scan done starting at the age of 50.
What does DXA scan result mean?
DXA scan reports your bone mineral density and its standard deviation from the norm (T-score) and standard deviation from your age group (Z-score):
T-score > -1 means normal bone density
T-score between -1 and -2.5 means Osteopenia, the stage before Osteoporosis
T-score <-2.5 means Osteoporosis
Z-score <-2 means that your bone mass is decreasing faster than expected and may indicate that you may have some secondary reasons for the bone loss
In patients who fall in osteopenic range, we can also calculate 10-year major osteoporotic fracture and hip fracture risk using FRAX tool.
When you see us for your bone health evaluation, we will review or order DXA scan and also order labs to make sure we exclude diseases that can cause bone loss and make sure that we can treat all the reasons for the bone loss.
We will also ask you about your supplements and diet. It is recommended that most of your calcium would come from the diet, but if you are not eating calcium rich diet, we will recommend additional calcium up to 1200 mg/day. We also will recommend vitamin D3 800 – 2000 IU/day supplementation unless more is needed to treat vitamin D deficiency.
Treatment
At your visit, we will review medication efficacy and safety as well how you take them.
We will also discuss the importance of fall prevention and exercise to prevent fractures.
Medical management for Osteoporosis can be divided into two groups: antiresorptive group and anabolic group.
Antiresorptive agents (bisphosphonates, denosumab, estrogen, SERMs) block the action of osteoclasts or “bone eating cells”.
Anabolic agents (teriparatide and abaloparatide) activate osteoblasts or “bone forming cells”. The newest addition to this group is romosozumab, that increases bone formation by inhibiting sclerostin.
For more information on Osteoporosis, please, visit nof.org
Calcium Disorders
Calcium is an element that is very precisely regulated in our bodies by our gut, kidneys and bones via parathyroid hormone.
A low calcium level (hypocalcemia) usually is caused by inadequate calcium absorption in the gut or by very severe lack of calcium in the diet. Vitamin D deficiency and “gut diseases” such as celiac disease can lead to calcium malabsorption. In rare cases, people are either born with or acquire deficiencies of parathyroid hormone that can lead to hypocalcemia.
A high calcium level (hypercalcemia) most commonly is caused by the benign (non-cancerous) tumor in parathyroid gland that is overproducing parathyroid hormone. Symptoms from hypercalcemia vary and correlate with the degree of calcium elevation. The higher calcium level, the more severe symptoms may be. Untreated, this disease can increase the risk for kidney stones and bone fractures. An evaluation needs to be done by a skilled endocrinologist and treatment most of the time is surgical.
Other causes for elevated calcium levels include medications, such as lithium and hydrochlorothiazide.
In some advanced cancer cases, patients also can develop hypercalcemia, especially if they develop bone metastases.
At Carolina Endocrine Associates we provide a comprehensive assessment and evaluation of the patient’s with calcium disorders and provide an individualized treatment plan. If surgery is indicated, we refer the patient to an experienced surgeon and follow the patient after surgery.